Clinical Compendium
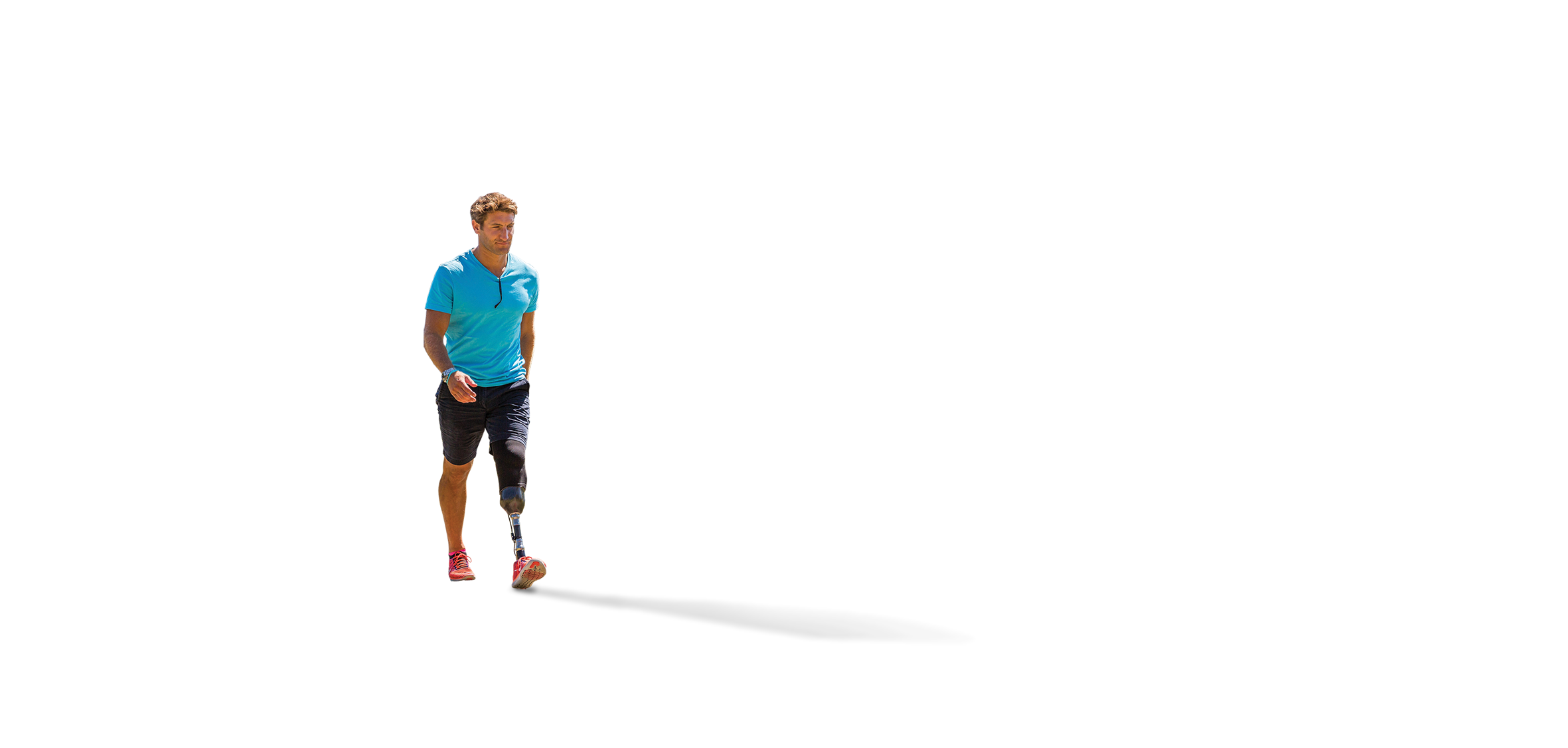
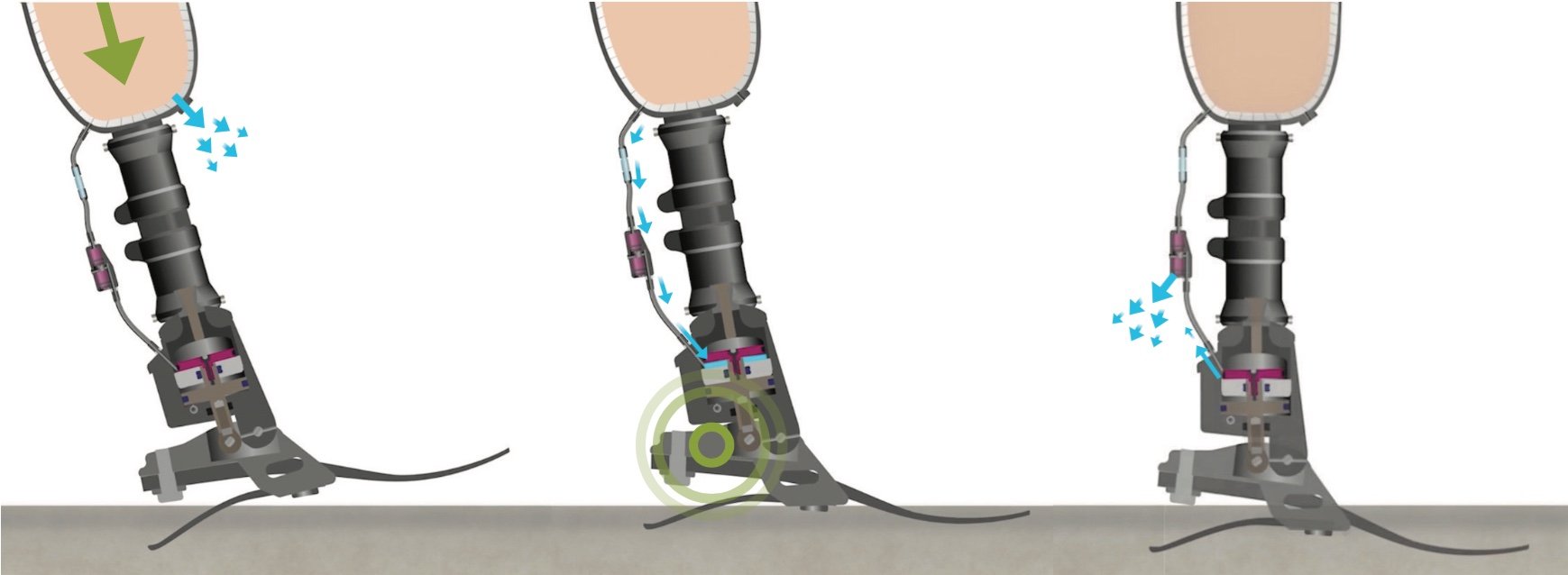
Blatchford Biomimetic Hydraulic Technology mimics the dynamic and adaptive qualities of muscle actuation to encourage more natural gait. Multiple independent scientific studies, comparing Blatchford hydraulic ankle-feet to non-hydraulic feet, have shown:
- Greater comfort, reduced socket pressures
- Improved safety, reduced risk of trips and falls
- Smoother, easier and more natural gait
- More evenly balanced inter-limb loading
- Greater satisfaction